2 Spermatogenesis & Oogenesis
- 2. SPERMATOGENESIS AND OOGENESIS
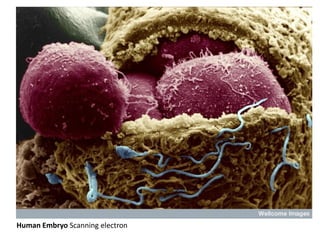
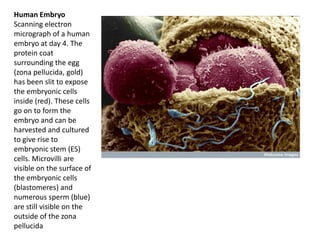
- 3. Human Embryo Scanning electron
- 4. Topics • Height lights • Structure of a mature spermatozoon • Spermatogenesis • Oogenesis • Ovulation • Abnormalities in formation of gametes
- 5. Height lights • Spermatozoon : head, neck, middle and principal piece. • Spermiogenesis = spermatid __spermatozoon. • Ovarian follicle. • Theca interna secrete estrogen. • ovulation.= process of shedding of the ovum. • Corpus luteum = is formed by enlargement and transformation of follicular cells, after shedding of the ovum. Secrete progesterone.
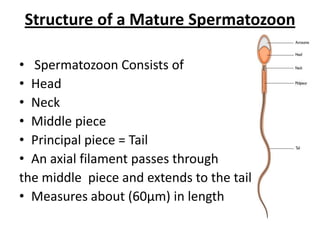
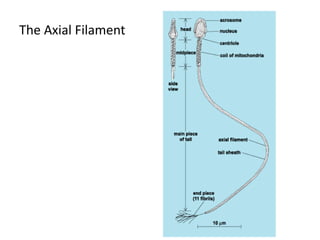
- 6. Structure of a Mature Spermatozoon • Spermatozoon Consists of • Head • Neck • Middle piece • Principal piece = Tail • An axial filament passes through the middle piece and extends to the tail • Measures about (60µm) in length
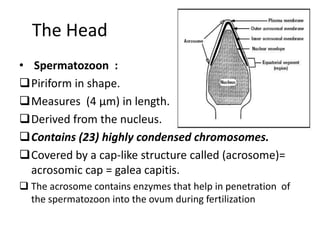
- 7. The Head • Spermatozoon : Piriform in shape. Measures (4 µm) in length. Derived from the nucleus. Contains (23) highly condensed chromosomes. Covered by a cap-like structure called (acrosome)= acrosomic cap = galea capitis. The acrosome contains enzymes that help in penetration of the spermatozoon into the ovum during fertilization
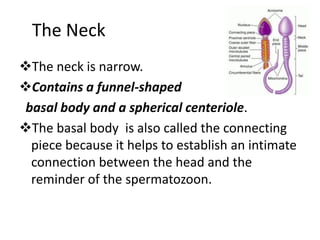
- 8. The Neck The neck is narrow. Contains a funnel-shaped basal body and a spherical centeriole. The basal body is also called the connecting piece because it helps to establish an intimate connection between the head and the reminder of the spermatozoon.
- 10. The Axial Filament Begins just behind the centeriole. Passes through the middle piece and most of the tail. Passes through the annulus (ring like structure at the point where the middle piece joins the tail). In the middle piece it is surrounded by a spiral sheath made up of mitochondria. Is composed of several fibrils. There is a pair of central fibrils, surrounded by nine pairs ( doublets ) arranged in a circle around the central pair. The whole system of fibrils is kept in position by a series of coverings.
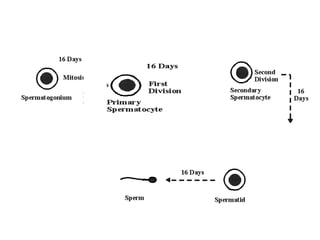
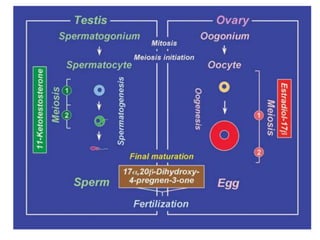
- 11. SPERMATOGENESIS o Takes place only during reproductive period, which begins at the age of puberty (12 to 16 years) and continues even through old age. o Spermatozoa are formed in the walls of the seminiferous tubules of the testis. o The various cell stages are as follows : 1. The spermatogonia type A or germ cells (44 + X+ Y) divide mitotically, to give rise to more spermatogonia type A and B. 2. The spermatogonia type B (44 +X + Y) enlarge, or undergo mitosis to form spermatocytes. 3. Primary spermatocytes (44 + X + Y) divide to form secondary spermatocytes. This is the 1st meiotic division. 4. Each secondary spermatocyte has (22 +X ) or (22 + Y) chromosomes. It divide to form two spermatids. This the 2nd meiotic division. 5. Each spermatid (22 + X or 22 + Y) gradually change its shape to become spermatozoon. This is called Spermiogenesis.
- 12. Spermiogenesis • Or spermateleosis • The process by which a spermatid becomes a spermatozoon. • The spermatid is amore or less circular cell containing a nucleus, Golgi apparatus, centeriole and mitochondria. all these components take part in forming the spermatozoon: 1. The nucleus forms ======================= head 2. The Golgi apparatus is transformed ======== acrosomic cap 3. The centeriole divides into two parts the axial filament appears to grow out of them • The process of Spermatogenesis , including Spermiogenesis, requires about two months for its completion
- 14. Maturation and Capacitation of Spermatozoa • When 1st seen in seminiferous tubules Spermatozoa : • are immature. • None motile. • Incapable of fertilizing an ovum. • Stored in the epididymis (undergo maturation). • Most of the cytoplasm is shed, but the cell membrane persist as a covering for the spermatozoon. • After maturation they acquire some motility (become fully motile only after ejaculation WHEN THEY GET MIXED WITH SECRETION OF THE PROSTATE GLAND AND SEMINAL VESICLES).
- 15. Maturation and Capacitation of Spermatozoa (continue) • ACQUIRE THE ABILITY to fertilize an ovum only after they have been in the female genital tract for some time. • This final step is called capacitation.( occurs in the uterus or uterine tube under the influence of substances secreted by female genital tract). • The glycoprotein coat and seminal proteins lying over the surface of the spermatozoon are altered.
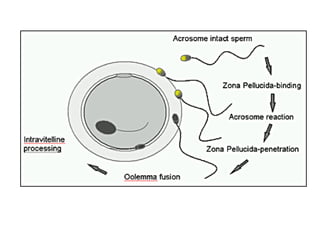
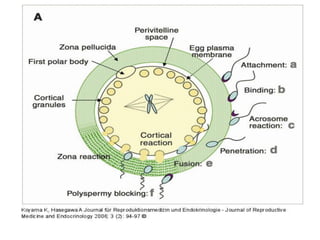
- 16. Maturation and Capacitation of Spermatozoa (continue) • Acrosome reaction: When spermatozoon becomes in contact with the zona pellucida, changes take place in the membrane of the acrosome and enable the release of lysosomal enzymes. • Zona reaction: some enzymes help in digesting the zona pellucida and in penetration of the spermatozoa through it.
- 18. Difference Between spermatogenesis and Spermiogenesis • Spermatogenesis is the complete process of formation of spermatozoon from a spermatogonium. • It includes the 1st + 2nd meiotic division + spermiogenesis. • Spermiogenesis is the process of transformation of a rounded spermatid into a spermatozoon.
- 19. OOGENESIS
- 20. OOGENESIS • Ovary is the female gonad. • It has an outer part called cortex. • It has inner part called medulla. • The cortex contains many oogonia. • All oogonia are produced at a very early stage (possibly before birth ) and do not multiply thereafter. • OOGENESIS is similar to spermatogenesis. However there important differences as well. (next slide).
- 21. Difference Between Spermatogenesis and Oogenesis One primary spermatocyte gives rise to 4 spermatozoa. • One primary oocyte forms only one ovum. When primary spermatocyte divides, its cytoplasm is equally distributed between the two secondary spermatocytes formed. • When the primary oocyte divides , almost all its cytoplasm goes to daughter cell, which form the secondary oocyte. • The other daughter cell (1st polar body), receives half the chromosomes of the primary oocyte, but almost no cytoplasm. • The 1st polar body is, therefore, formed merely to get rid of unwanted chromosomes.
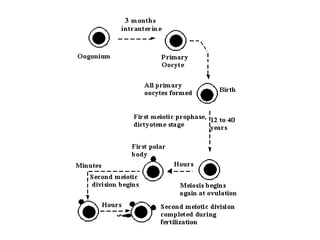
- 22. Further Details !!!!!!!!!!!!!!!!!!!!! • Only 400 ova are discharged During the entire reproductive life of a female , (400 out of 40,000). • 5 to 30 primary oocytes start maturing each menstrual cycle, but only one of them reaches the maturity and is ovulated. • In late fetal period primary oogonia enlarged to form primary oocytes. • At the time of birth all primary oocytes are in the prophase of the 1st meiotic division. There number is about 40,000. • The primary oocytes remain in prophase and do not complete their 1st meiotic division until they begin to mature and are ready to ovulate.
- 23. Further Details (continue) • The reproductive period of a female is between 15 to 50 years of age. • With each menstrual cycle, a few primary oocyte (about 5 to 30 ) begin to maturate and complete 1st meiotic division shortly before ovulation. • The 1st meiotic division of primary oocyte produces two unequal daughter cells. Each cell has the haploid number of chromosomes (23). The large cell is called the secondary oocyte, and the smaller one called the 1st polar body. • The secondary oocyte immediately enters the second meiotic division. Ovulation takes place while the oocyte in metaphase. The secondary oocyte remains arrested till fertilization occurs.
- 24. Further Details (continue) • The second meiotic division is completed only if the fertilization occurs. • This division results in two unequal daughter cells. • The smaller cell is called the 2nd polar body. The 1st polar body may also divide during the 2nd meiotic division. • If fertilization does not occur, the secondary oocyte fails to complete the 2nd meiotic division, and degenerates in about 24 hours after ovulation
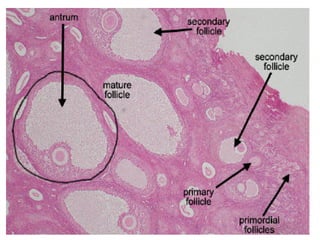
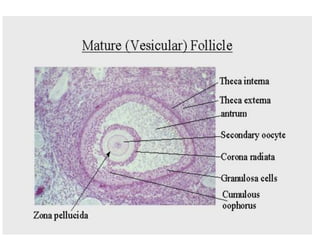
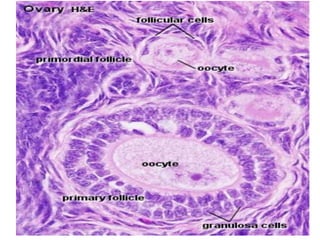
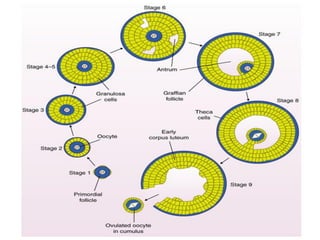
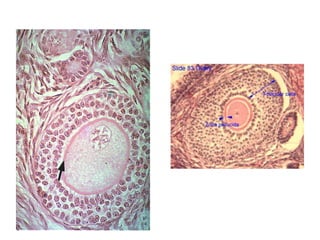
- 25. Formation of Ovarian Follicles • Ova develop from oogonia. • Then oogonia are surrounded other cells that form the stroma. • These stromal cells form ovarian or graafian follicles that surround ova and protect them. • The stages in the formation of follicle are as follows: 1. Follicular cells: some cells of the stroma become flattened and surround an oocyte. These flattened cells from the ovarian follicle and, therefore, called follicular cells. 2. Primordial cells: the flattened follicular cells become columnar. 3. Zona pellucida: a homogenous membrane appears between follicular cells and oocyte. 4. Membrana granulosa: the follicular cells proliferate to form several layers these constitute the Membrana granulosa and the cells called granulosa cells.
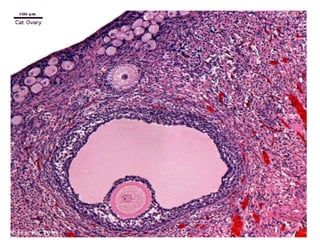
- 30. The stages in the formation of follicle are as follows (continue1) 5. Antrum: a cavity appears within the membrana granulosa. With its appearance a follicle is formed. 6. Cumulus oophoricus: or cumulus ovaricus • The cavity of the follicle rapidly increases in size. • The wall of the follicle becomes thin. • The oocyte lie eccentrically in the follicle, surrounded by some granulosa cells that are given the name Cumulus oophoricus or cumulus ovaricus . • The cells that attached to the wall of the follicle are given the name discus proligerus.
- 31. The stages in the formation of follicle are as follows (continue2) 7. Theca interna: • as the follicle expands, the stromal cell surrounding the membrana granulosa become condensed to form a covering called (theca interna). • The cells of the theca interna later secrete a hormone called estrogen; and they are called the thecal gland. 8.Fully formed ovarian follicle: • Outside the theca interna some fibrous tissue becomes condensed to form another covering for the follicle called the theca externa.
- 32. Inter-dependence of Oocyte and Follicular cells • The follicular cells secrete meiotic inhibitory factors. • These factors prevent primary oocytes from maturing beyond the prophase of the 1st meiotic division. This effect may last for many years. • The follicular cells are also responsible for growth metabolism and maturation of oocytes. • Conversely, the oocytes are responsible for proliferation and differentiation of follicular cells. factors produced in the oocyte help in the formation and maturation of graafian follicles.
- 33. Ovulation • The shedding of the ovum from the ovary is called ovulation. • The ovarian follicle is at first very small compared to the thickness of the cortex of the ovary. • As it enlarges, it reaches the surface and the form a bulging. • Ultimately the follicle ruptures and the ovum is shed from the ovary. • Just before ovulation: • The follicle may have a diameter of 15mm. • The stroma and theca become very thin. • An a vascular area (stigma) appears over the most convex point of the follicle. • AT THE SAME TIME, THE CELLS OF THE CUMULUS OOPHORICUS BECOME LOOSENED BY ACCUMULATION OF INTRACELLULAR FLUID BETWEEN THEM.
- 34. FACTORS LEAD TO OVULATION 1. High LH (luteinizing hormone) concentration. 2. Increase activity of collagenase enzyme. (digest the collagen fibers surrounding the follicle). 3. Increase prostaglandins concentration (results in smooth muscle contraction). 4. Increase pressure of fluid in the follicular cavity. 5.Enzymatic digestion = the main factor responsible for ovulation.
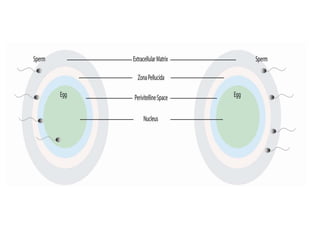
- 35. Structure of the Ovum • Shed ovum is not fully mature . • It is surrounded by zona pellucida. • Some cells of zona radiata can be seen sticking to the outside of the z. pellucida. • It is in fact a secondary oocyte that is undergoing division to shed off the 2nd polar body. • No nucleus ( nuclear membrane dissolved for the 2 nd meiotic division). • A spindle is present.
- 37. Structure of the Ovum (continue) • A distinct perivitelline space is seen between the cell membrane (vitelline membrane) and the zona pellucida. • The 1st polar body lies in this space (perivitelline space). • The ovum is a very large cell and measures 100µm. (most other cell body measure less than 10µm). One mm = 1000 µm One meter = 1000 mm
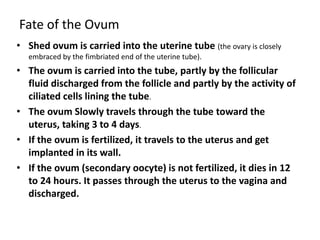
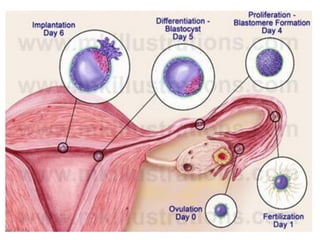
- 39. Fate of the Ovum • Shed ovum is carried into the uterine tube (the ovary is closely embraced by the fimbriated end of the uterine tube). • The ovum is carried into the tube, partly by the follicular fluid discharged from the follicle and partly by the activity of ciliated cells lining the tube. • The ovum Slowly travels through the tube toward the uterus, taking 3 to 4 days. • If the ovum is fertilized, it travels to the uterus and get implanted in its wall. • If the ovum (secondary oocyte) is not fertilized, it dies in 12 to 24 hours. It passes through the uterus to the vagina and discharged.
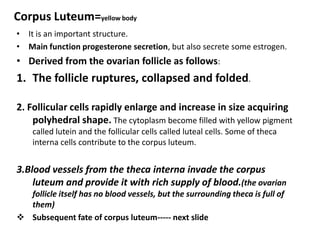
- 41. Corpus Luteum=yellow body • It is an important structure. • Main function progesterone secretion, but also secrete some estrogen. • Derived from the ovarian follicle as follows: 1. The follicle ruptures, collapsed and folded. 2. Follicular cells rapidly enlarge and increase in size acquiring polyhedral shape. The cytoplasm become filled with yellow pigment called lutein and the follicular cells called luteal cells. Some of theca interna cells contribute to the corpus luteum. 3.Blood vessels from the theca interna invade the corpus luteum and provide it with rich supply of blood.(the ovarian follicle itself has no blood vessels, but the surrounding theca is full of them) Subsequent fate of corpus luteum----- next slide
- 42. Subsequent fate of corpus luteum • Subsequent fate of corpus luteum depends on whether the ovum is fertilized or not: If the ovum is not fertilized, the corpus luteum persist for 14 days. • During this period it secretes progesterone. • It remains small and is called corpus luteum of menstruation. • At the end of functional life, it degenerates and form a white fibrous mass called the corpus albicans (white body).
- 43. Subsequent fate of corpus luteum (continue) If the ovum is fertilized and pregnancy results, • The corpus luteum persists for 3 to 4 months. • This larger than corpus luteum of menstruation and called the corpus luteum of pregnancy. • The C. luteum of pregnancy may occupy one-third to half the total volume of the ovary. • The progesterone secreted by it is essential for the maintenance of pregnancy in the 1st few months • After the fourth month, the corpus luteum is no longer needed, as the placenta begins to secrete progesterone.
- 44. Subsequent fate of corpus luteum (continue) • Human chorionic gonadotropin hCG secreted by the trophoplast cells of the developing embryo prevent degeneration of the corpus luteum of pregnancy. • The series of changes that begin with the formation of an ovarian follicle and end with the degeneration of the corpus luteum is called the ovarian cycle.
- 45. Fate of the Ovarian Follicles • In each cycle only one follicle reaches maturity, and becomes a corpus luteum. • At the same time several other follicles also begin to develop, • But do not reach maturity. • These follicles do not persist into the next ovarian cycle, but undergo degeneration. • The ovum and granulosa cells of each follicle disappear. • Theca interna cells proliferate to form the interstitial glands (corpus atretica). • These glands are believed to secrete estrogens. • After period of activity, each gland becomes a mass of scar tissue indistinguishable from the corpus albicans formed from the corpus luteum.
- 46. Differences between Male and Female Gamete • Motility • Size and shape • Cytoplasm • Chromosomal type
- 48. Reproductive Period Puberty begins 10 to 14 years • Female • Male Continue • Female 45 to 50 years • Male till death average sixth decade
- 49. Viability of Gametes • Ovum degenerate 24hours after ovulation. • At most it may survive for 2 days. • Sperm degenerate 48hours after ejaculation • May survive up to 4 days in female genital tract (submucosal)
- 50. Abnormality in Formation of Gametes 1.Abnormality of form. 2.Chromosomal Abnormality. 3.Gene abnormalities (mutation)
- 51. Abnormality of form. Spermatozoa: • Too large = giant. • Too small = dwarf. • The head, body or tail may be duplicated. The ovum: • Unusually large nucleus. • Two nuclei. • Two oocytes in one follicle.
- 52. Gene abnormalities (Gene mutation) • Genes are responsible for normal embryological development. • A change in the structure of a gene may occur at the time of gametogenesis. This may give rise to birth defect. • The change in the structure or function of a gene is called gene mutation. • At present many birth defects are known which are caused by gene mutations.
- 53. Chromosomal Abnormality The gametes may be abnormal in chromosomal content as follows During the 1st meiotic division, the two chromosomes of a pair, instead of separating at anaphase, may go both to the same pole. (this is called non-disjunction).= 24 chromosomes. At fertilization the zygote will have 47 chromosomes (3 identical chromosomes). =trisomy. For example Down syndrome (mongolism). Sex chromosome may be abnormal : XXX = SUPER FEMALE ???????? XXY = KLINEFELTER’S SYNDROME abnormal male.
- 54. Chromosomal Abnormality (continue)1 One both chromosomes of a pair go to one gamete, the other gamete has only 22 chromosomes. And at fertilization the zygote has only 45 chromosomes. Here one pair is represented by one chromosome, this is called monosomy (Turner syndrome = one X and absent Y chromosome).
- 55. Chromosomal Abnormality (continue)2 MORE THAN ONE PAIR MAY BE AFFECTED. one pair may be represented by more than 3 chromosomes, when this happens with sex chromosomes, individuals with the constitution XXXY XXXXY XXYY XXXX SOME GAMETES HAVE DIPLOID NUMBER SO the zygote will have 46 + 23 = 69 (triploidy), higher multiples of 23 may be seen.
- 56. Chromosomal Abnormality (continue)3 Cross over abnormalities: 1. Translocation . 2. Deletion. 3. Duplication and missing. 4. Inversion. Isochromosomes and Mosaicism.
- 60. Human Embryo Scanning electron micrograph of a human embryo at day 4. The protein coat surrounding the egg (zona pellucida, gold) has been slit to expose the embryonic cells inside (red). These cells go on to form the embryo and can be harvested and cultured to give rise to embryonic stem (ES) cells. Microvilli are visible on the surface of the embryonic cells (blastomeres) and numerous sperm (blue) are still visible on the outside of the zona pellucida